Researchers 3D bioprint breast cancer tumors and treat them in new study
Researchers at Penn State have successfully 3D bioprinted breast cancer tumors and treated them in a breakthrough study to better understand the disease that is one of the leading causes of mortality worldwide.
A scientific first, the achievement lays the foundation for precision fabrication of tumor models. The advancement will enable future study and development of anti-cancer therapies without the use of "in vivo" — or "in animal" — experimentation.
“This will help us understand how human immune cells interact with solid tumors,” said Ibrahim Ozbolat, senior author of the study. “We’ve developed a tool that serves as a clinical test platform to safely and accurately evaluate experimental therapies. It is also a research platform for immunologists and biologists to understand how the tumor grows, how it interacts with human cells, and how it metastasizes and spreads in the body.”
Ozbolat specializes in 3D printing to create a range of tissues for use in human healthcare. The lab’s U.S. National Science Foundation-supported work using 3D bioprinting to help in the study of breast cancer was recently published in Advanced Functional Materials and Biofabrication.
The researchers used a relatively new technique called aspiration-assisted bioprinting to precisely locate tumors in three dimensions and create the tissue. The researchers then formed the tissue into a multi-scale vascularized breast tumor model with blood vessels, which they discovered responded to chemotherapy and cell-based immunotherapeutics.
The team first validated the accuracy of its tumor model by treating it with doxorubicin, an anthracycline-based chemotherapeutic drug commonly used for treating breast cancer. Finding that the 3D printed tumor responded to chemotherapy, the researchers went on to test a cell-based immunotherapeutic treatment on the tumor in collaboration with Derya Unutmaz, an immunologist at Jackson Laboratory.
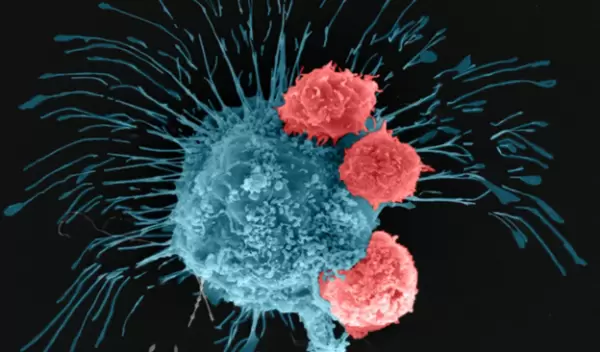
The researchers used human CAR-T cells that were engineered via gene editing to recognize and fight an aggressive form of breast cancer cells. After 72 hours of circulating the edited CAR-T cells through the tumor, the researchers found that the cells within the bioprinted tumor had generated a positive immune response and were fighting off the cancer cells.
