Rethinking computerized clinical alerts
June is National Safety Month, with a call to action to reduce harm and injury through enhanced attention to safety.
Healthcare in the United States is constantly evolving to provide safe and quality care while decreasing the incidence of medical errors. Advances in health information technology can improve patient safety, including in the area of safer prescribing of medications through the smarter design of clinical alerts.
A frequent source of errors in clinical care settings is related to the prescribing of medications. Electronic Health Records have the potential to improve safety by notifying providers of potentially harmful medication interactions. Currently, clinicians using electronic health records encounter numerous alerts as they navigate computerized prescribing for their patients.
While these alerts are critical for patient safety, they are often overridden or ignored due to "alert fatigue"--an unintended consequence of the computerization of health care, where clinicians become desensitized to the large volume of safety alerts.
An estimated 90 percent of drug interaction alerts are ineffective, as they temporarily halt prescribing with generic warning imagery and brief messaging, but do not offer user-friendly interfaces with advice that resonates with the prescriber.
With support from the National Science Foundation's (NSF) Smart and Connected Health Program, Davide Bolchini and Jon Duke from Indiana University-Purdue University Indianapolis (IUPUI) are advancing knowledge in Human Computer Interaction (HCI)--a field that studies the design, development and implementation of information technologies for optimal use by a target audience--through a collaborative project to rethink and redesign computerized clinical alerts.
Identifying disconnects
"Although physicians routinely encounter drug-drug interaction alerts during daily medication prescribing, the effectiveness of such alerts remains extremely low," explained Duke, director of drug safety informatics at Regenstrief Institute.
An additional barrier to the desired effect of alerts is that healthcare providers may be wary of utilizing computerized advice in the same way they would trust advice from medical literature or peer providers.
These challenges necessitate new approaches to design which can leverage health information technology to improve the care team's integration of information into computerized alerts to ensure patient safety. Multiple, complex factors influence the healthcare team's decision-making and the researchers want to integrate this knowledge to optimize the design and impact of computerized drug interaction alerts.
The overarching objective is to re-design the content and visualization of alerts such that they capture the attention of providers while offering advice more likely to be trusted than current alerts.
"We are looking at how to improve the trust between the physician and computer," said Duke.
Visualizing trustworthy alerts
A crucial step in the process of transforming the design of drug-drug interaction alerts involved studying the types and sources of information that providers deemed important and impactful.
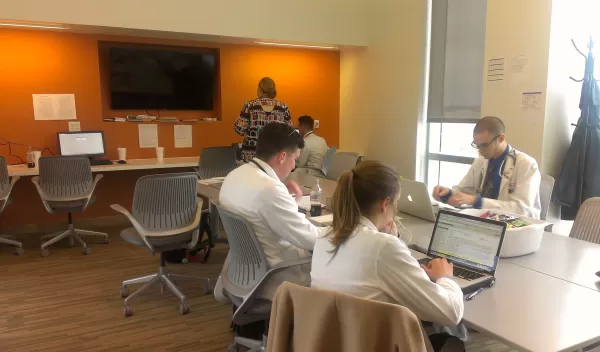
The team researched information flow by directly observing hospital team meetings. They then constructed work models to identify the themes that drive trusted advice in clinical settings. The models integrated the roles of evidence in medical literature and advice provided by peer consultants such as pharmacists and subspecialists.
The research team is now actively using this foundational knowledge to transform the computer interface to reflect various models of trust based alerts.
The team is also developing novel interface designs where computer alerts can convey drug safety guidance in various forms, including changes in the alert message tones, such as from danger-based tones to supportive ones. The new alert designs also vary the source of knowledge from the empirical medical research to a peer collaborator.
The design ideas include visualizations for different trust-based alert messages. Examples include warnings whose message stresses empathy, peer-endorsement, conflict-mitigation and collaboration. The team will test and evaluate the different alerts in the lab and in hospital environments to determine the effect on prescriber responses. They will also elicit healthcare provider feedback on the visual aspects and impact of the alerts.
"This innovative Human Computer Interaction project illustrates how studying novel visualizations and design can better integrate information that is meaningful to clinicians and maximize the potential of computerized alerts to improve safety," said Wendy Nilsen, Smart and Connected Health program director at NSF.
The broader impacts of this Smart and Connected Health project are numerous. The team believes that translating these research findings into real-world electronic medical record systems could improve the user experience of prescribers and yield a potential reduction in the millions of adverse drug events that occur each year.
"A key aspect of the work is to generate alerts that are perceived as collaborating with the providers rather than critiquing every micro-decision," said Bolchini. "We have the opportunity to change technologies which are pervasive and create the next generation of systems for human use and patient safety."
