Synthetic platelets stanch bleeding, promote healing using advanced materials
A research team has developed synthetic platelets that can stop bleeding and enhance healing at the site of an injury. They demonstrated that the synthetic platelets work well in some animals but have not yet begun clinical trials in humans.
The findings were supported in part by the U.S. National Science Foundation and published in the journal Science Translational Medicine.
"We've developed synthetic platelets that can be used with patients of any blood type and are engineered to go directly to the site of injury and promote healing," says Ashley Brown, a member of the research team and associate professor in the joint biomedical engineering program at North Carolina State University and the University of North Carolina at Chapel Hill. Brown received an NSF Faculty Early Career Development Program award to explore the development of advanced materials that can mimic the wound-healing abilities of natural platelets.
Many medical situations require platelet transfusions, such as patients with severe bleeding or receiving chemotherapy. Currently, platelets only come from blood donors, ideally those with a compatible blood type. However, human platelets are in short supply, have a limited shelf life, and must be stored under controlled conditions.
"The synthetic platelets are also easy to store and transport, making it possible to give the synthetic platelets to patients in clinical situations sooner — such as in an ambulance or on the battlefield," says Brown.
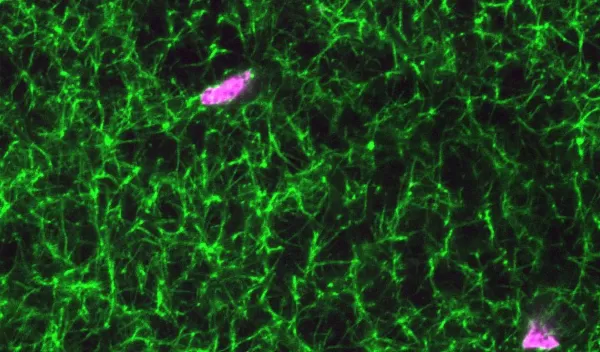
The synthetic platelets are made of hydrogel nanoparticles that mimic the size, shape and mechanical properties of human platelets. Research in mice and pigs demonstrated that the synthetic platelets traveled to the site of a wound, expedited successful clotting without problems and accelerated healing.
The researchers are continuing their testing and expect to obtain Food and Drug Administration approval to begin clinical trials within two years.
